All information about ectopic pregnancy on this page is given for research purposes only. This information is not given as a substitute for your personal care and diagnosis by a licensed physician. Under any and all circumstances, if you think that you may have an ectopic pregnancy, consult your physician immediately. Always insist that your medical professionals take your concerns seriously.
What Is Ectopic Pregnancy?
Ectopic pregnancy, also known as a tubal pregnancy, is a potentially life-threatening form of pregnancy in which implantation of the fertilized egg occurs outside the uterus. About 97% occur in the fallopian tube. The remainder implant in the abdominal cavity, on the ovary, or within the cervix.
Heterotopic pregnancies occur in one of these areas, while there is also a pregnancy in the uterus. Approximately 100,000 ectopic pregnancies occur each year. Approximately 1 in 66 women will experience this type of pregnancy.
Ectopic pregnancy is a very serious condition. When the pregnancy grows in these abnormal areas, it can easily cause massive, rapid bleeding, and even death.
What Causes Ectopic Pregnancy?
The most likely reason for the occurrence of an ectopic pregnancy, is a ruptured Fallopian tube. This can be due to a number of things:
- history of pelvic inflammatory disease (PID) or other sexually transmitted diseases-which accounts for about 30-50% of all ectopic pregnancies (ampulla damage)
- history of pelvic surgery (scar tissue outside the tube may causes constriction on the tube)
- history of tubal surgery
- fertility being restored through the reverse of tubal ligation
- tubal ligation itself
- tumors or cysts in the tubes
- fibroids in the uterus (which block the tube’s entrance into the uterus)
- endometriosis of the fallopian tube
- smoking (may damage the ampulla of the fallopian tube)
- assisted reproduction techniques (IVF, GIFT, ZIFT, superovulation)
- history of ectopic pregnancy
- congenital defects in the structure of the tubes (e.g. exposure to diethylstilbestrol (DES) in utero)
- hormonal imbalance (excessive levels of progesterone or estrogen may interfere with the contractions of the fallopian tube)
- there is also a slightly increased risk of a pregnancy being ectopic in the case of a women conceiving while having an intra-uterine contraceptive device (IUD) in place. While there is a higher percentage of ectopic pregnancy in IUD users, the IUD does not cause it. Rather, it functions to prevent uterine pregnancies, so that any fertilization that does occur results in an ectopic pregnancy
“Ampulla” are the nodes inside the fallopian tube that push the embryo down into the uterus. You CAN NOT cause yourself to have an ectopic pregnancy. If possible, avoid the risks factors before you get pregnant. You may be able to significantly decrease your chances of having an ectopic pregnancy. However, an ectopic pregnancy is not always the result of an obvious defect. It can be a “fluke”–most women who are diagnosed with an ectopic pregnancy do not have a recognizable risk factor or diagnosis. Pray that this is true in your case, but please take all cautionary measure available before attempting to conceive again.
What Are The Maternal Risks Of Ectopic Pregnancies?
They are the second leading cause of pregnancy-related deaths in the first trimester and account for 9% of all pregnancy-related deaths in this country.
If left untreated, an ectopic pregnancy may be potentially life-threatening, as there is a chance of the tube bursting, resulting in serious and life threatening internal bleeding.
Ectopic pregnancy symptoms can be hard to identify
This condition often mimics a late menstrual cycle. Irregular vaginal bleeding is another sign. Furthermore, abdominal pain may be present. Shoulder pain is another possible symptom. Rectal pressure is also linked to it. Yet, some women might not show any specific signs. In these cases, it’s challenging to diagnose. Thus, it appears just like a regular pregnancy.
Can I risk another pregnancy after a previous ectopic pregnancy?
A sensitive pregnancy test (HCG) can determine whether a normal pregnancy is “healthy” or not.Women carry risk factors for ectopic pregnancy. Some have a previous history. Others show more severe symptoms. Therefore, these women need careful monitoring. This monitoring uses HCG blood tests. Firstly, a test is conducted roughly 12 days after conception. Next, further tests follow up to 5-6 weeks after conception.In a healthy pregnancy, HCG levels rise steadily. Specifically, they increase about 66% every two days. However, an ectopic pregnancy might be indicated by different patterns. Particularly, if these levels fail to rise correctly, it raises suspicion.
In addition to HCG tests, pelvic ultrasound is often helpful. Specifically, it determines if a pregnancy exists within the uterine cavity. It confirms the presence or absence of a pregnancy in the uterus.
Approximately 5-6 weeks after the last menstrual period, the use of ultrasound can determine if there is a gestational sac in the uterus. The ultrasound may even detect fallopian tube ruptures or the presence of a pelvic mass, representing an ectopic pregnancy.
Ask for a printout or a copy of the ultrasound. You may later be glad that you did!
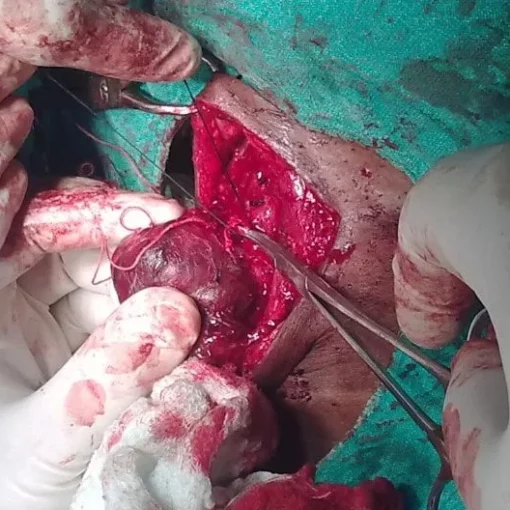
If an ultrasound doesn’t detect an ectopic pregnancy, laparoscopy is a better alternative. This procedure uses a small, lit camera. It is inserted through tiny incisions below the navel or near the pubic bone. Today, early diagnosis and treatment of ectopic pregnancy is possible. It helps to avoid tubal rupture in 80 percent of cases.
So, what happens when an ectopic pregnancy is diagnosed?
Unfortunately, even a viable ectopic fetus cannot survive. Interestingly, a quarter of such pregnancies self-resolve before confirmation. After diagnosis, we must consider treatment options. Emergency surgery is sometimes necessary to manage severe internal bleeding.
Alternatively, if we detect the condition early and the tube hasn’t ruptured, we can opt for medical management. If the pregnancy remains unruptured, Methotrexate is a viable option. This drug inhibits the rapid cell division in early pregnancy.
The administration of Methotrexate may require multiple injections. Subsequently, close monitoring of HCG levels in the blood is essential. However, Methotrexate is not a one-size-fits-all solution. Finally, we need to track HCG levels to ensure they decrease appropriately.
The HCG level should return to zero in approximately four weeks. Side effects (diarrhea, mild irritation of the mouth or stomach, elevated liver enzymes) occur in about 4% percent of women treated with Methotrexate. Methotrexate may fail to resolve the ectopic pregnancy, and tubal rupture may occur. However, with careful monitoring, rupture may be avoided. The advantages of Methotrexate therapy include less tubal damage, less expense, and an increase in the possibility of future fertility.
NOTE:
New studies indicate that high blood levels of folic acid can interfere with methotrexate. Consequently, if you have an ectopic pregnancy, avoid prenatal vitamins. When additional findings emerge, we’ll update you.
Often, emergency rooms diagnose ectopic pregnancies. Women usually present severe symptoms such as pelvic pain and potential dizziness. In most cases, these symptoms result from the tube’s rupture and significant internal bleeding. As a result, a more invasive surgery becomes necessary. Typically, this procedure may involve removing the entire tube. However, it rarely necessitates the removal of the ovary.

Removal of the Fallopian Tubes?
In a laparotomy, a surgeon creates a 5 cm incision on the lower abdomen. Subsequently, they may opt for one of three procedures. First, there’s a salpingostomy, where the pregnancy is removed through a small cut in the tube wall. After this, the tube is mended.
Alternatively, they might choose a Tubocornual Anastomosis. In this case, the surgeon removes the tube section with the ectopic. Then, they reconnect the remaining tube to the uterus.
Lastly, a Tubotubal Anastomosis is another possible procedure. Here, the surgeon cuts out a tube section. Following this, they sew the two severed pieces back together.
However, there is data suggesting that repaired tubes have a higher rate of recurrent ectopic pregnancy (in the same tube). A salpingectomy (removal of the Fallopian tube, if the ectopic has already caused irreversible damage to the tube or the tube has burst) may be necessary.
In some cases, wherein the pregnancy has embedded itself into the uterus, a hysterectomy is necessary. However, this is the exception, and NOT the rule.
Sadly, the resolution has no happy ending. However, there is research being done on the movement of an ectopic pregnancy into the uterus. The data on this research is “sketchy”, but when conclusive information is available, I will include in in this section.
What About Subsequent Pregnancies?
Your recovery time from the “resolution” of an ectopic pregnancy depends upon what type of procedure was performed. Your physician will be able to give you a time line regarding your future attempts at conception.
There are no statistics (regarding subsequent pregnancies by natural conception) given in this section for several reasons: data changes from study to study, the results of these studies are hard to interpret (when compared to others), and every woman’s body is different. I may later provide results from several independent studies, if I receive numerous requests for such data.
There is a possibility that you may have another ectopic pregnancy (estimated at a 12% recurrence rate), therefore your next pregnancy would need careful monitoring-HCG testing and ultrasound scanning in the early weeks of a pregnancy will offer peace of mind.
If you have undergone a salpingectomy and provided the other tube is normal, there is still a good chance of conception taking place, although it may take a little longer.
Precautionary tests after an ectopic pregnancy
There are precautionary tests that should be done prior to conceiving again after an ectopic pregnancy. Your physician might recommend one of the following.
We recommend that you consider consulting with a Reproductive Endocrinologist (R.E.), who may be better able to assist you in getting pregnant in the future. An R.E. not only provides assisted reproductive technologies. They are educated in the field and can perform the testing necessary to predict possible future ectopic pregnancies. Most insurance companies cover the cost of diagnostic testing (especially after an ectopic). Be sure to check with your insurance provider before making an appointment, if you will not be able to pay the consultation fee(s).
Diagnostic Testing Options
- Hysterosalpingogram (HSG) involves inserting a dye into the uterus. The dye is usually iodine-based. A catheter is used for this procedure. It is inserted through the vagina. X-ray makes the uterus and fallopian tubes visible.This method can uncover uterus abnormalities. It can also show blockages in the fallopian tubes. A condition called hydrosalpinx can be detected too. In a perfect scenario, the dye should flow out smoothly. It should pass through the fallopian tubes and into the abdominal cavity.However, complications can occur. One possible complication is infection. Fortunately, infections are infrequent. They are potential risks for any procedure involving foreign substance insertion. These substances are introduced into the reproductive tract. Side-effects can also be experienced. These may include cramping and vaginal bleeding.
- Sonohysterography (SHG) is similar to HSG. It also uses a catheter to insert liquid into the uterus. The liquid is often saline-based. This procedure also allows visualization of the uterus and tubes, but via ultrasound.Just like with HSG, the liquid should flow out easily. It should move from the fallopian tubes into the abdominal cavity. Infections are potential complications. These are rare, however. Again, any procedure involving a foreign substance presents such risks. SHG side-effects might include cramping and bleeding.
While the HSG and SHG are similar in purpose and performance, the SHG can be more expensive. This may be due to the use of the ultrasound instead of the x-ray. Be sure to check with your insurance provider (to confirm coverage) before scheduling. The SHG has benefit for those who may be allergic to iodine. Also, the SHG involves no exposure to x-ray. However, with both the HSG and SHG, the condition of the lining of the fallopian tube is not apparent. The lining of the fallopian tube “coaxes” the embryo down into the uterus, and damage to the lining may prevent it from doing so.
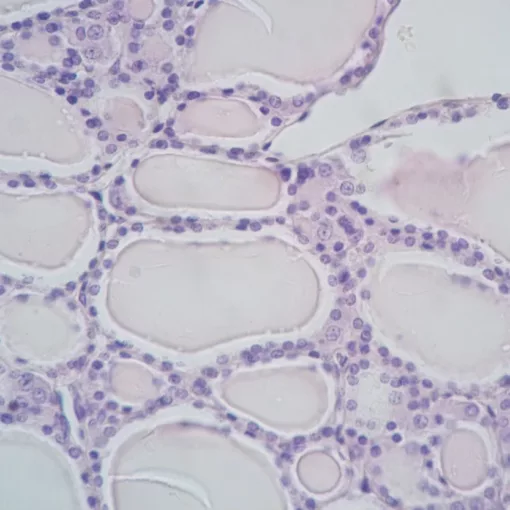
- Falloscopy (performed in conjunction with a laporoscopy): a scope is inserted into the fallopian tube (through the fimbria) to examine the lining. The lining of a healthy fallopian tube looks like a small mountain range of projecting, moving nodes. Areas without nodes or damaged nodes (flat and/or non-moving), indicate risk for ectopic pregnancy.
Indeed, HSG, SHG, and falloscopy can have therapeutic effects. Sometimes, these tests can clear minor blockages in the fallopian tube. Consequently, fertility might increase. Yet, there is a risk. Unintentional pregnancy dislodging may occur during these tests. Thankfully, this risk can be mitigated. How? By performing these tests after a menstrual period. Furthermore, combining them with HCG urine and blood tests can help. Therefore, careful timing and testing can reduce this risk significantly.
Corrective Surgeries
First of all, corrective surgeries exist for a damaged fallopian tube. Interestingly, these may not have been fully repaired during diagnosis. Specifically, this refers to the diagnosis or removal of an ectopic pregnancy. Consequently, additional surgeries become necessary for complete repair. Based on my research, data on these surgeries is inconclusive pertaining to success (future pregnancy rate) and rate of future ectopic (in the damaged/repaired tube). Discuss these options with your physician. For more information on corrective surgery of the fallopian tube, visit ivf.comIf your doctor has given you the “go ahead” to attempt to conceive naturally, keeping track of your cycles by charting your temperature with a basal thermometer is a valuable tool. Taking Charge of Your Fertility by Toni Weschler, MPH explains the charting process, other ovulatory signs, and provides wonderful information about a woman’s cycle in general. I learned a lot from this book!
Some women who have suffered an ectopic pregnancy will not be able to conceive naturally again. This is sometimes true for women in whom both fallopian tubes were left intact. Unfortunately, the reasons are for this infertility are not always determinable.
When preparing for another pregnancy, learn all that you can about your body and what may lie ahead for you.
Those considering adoption should consider seeking qualified, licensed counsel to determine if adoption is right for them and to emotionally prepare themselves for an adoption. Should you decide that adoption is right for you, we also urge you to seek the services of a licensed attorney.
Ask questions of qualified personnel. If you feel that your questions are not being answered, change personnel. This is your body, and your life. Hurting someone’s feelings (by changing physicians, counselors, attorneys) should not be an issue.